MELANOMA IN SITU OF BACK

HISTORY
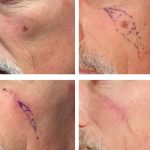
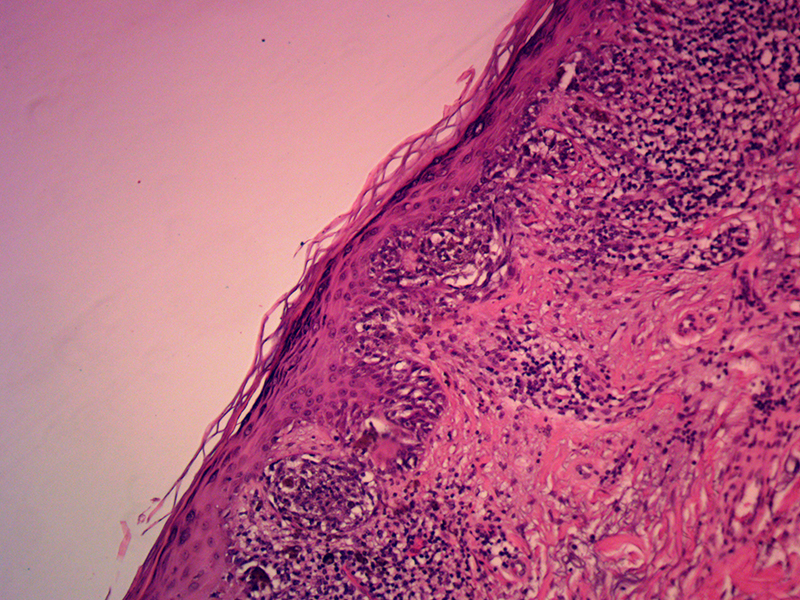
69-year-old man presents with melanoma in situ of the upper back. A biopsy on 6/15/2017 showed malignant melanoma at least in-situ and at least Clark’s level I with margins involved. Excision and skin graft closure performed on 8/9/2017. Pathology showed residual malignant melanoma in situ with involved margin at 2-4 o’clock.
DISCUSSION
Management of indistinct margins of a melanoma in situ is a challenge. This case represents an optimistic management model where skin graft reconstruction is performed at the time of excision with 5mm margins. Excising with wider margins can result in significantly larger defect with more difficulty with healing and closure. More conservative 5 mm margin excision with delayed additional margin excision is possible. A crescent excision of the involved area can be closed directly with the edge of the skin graft. This skin graft can survive the additional tension two to three weeks after initial grafting.
The classic management model is leaving the wound open until the margins are verified as clear. The reconstruction is performed at the second stage. If margins are not clear, then additional margin excision and simultaneous reconstruction can be performed at the second stage. The disadvantage of this approach is the open wound that the patient has to endure. A modification of the classic approach involves placing a porcine xenograft on the wound. This avoids a skin graft donor site closure as was the case on this patient’s right neck. The xenograft allows for less crusting and less symptomatic healing as compared to an open wound. Of course, the xenograft requires secondary intention healing that would take place over the following six to eight weeks. The skin grafts advantage is rapid healing.
Of course, the best closure technique in this area is direct wound closure. In larger wounds and in inherently high tension areas, direct closure can result in wound dehiscence and significant scar widening.