Is there a Role for Sentinel Lymph Node Biopsy in Cutaneous Squamous Cell Carcinoma?
Sentinel lymph nodes are defined as the first lymph nodes that receive metastases from a primary tumor. The concept of a first echelon node was first described by Seaman and Powers and later given the name “sentinel node” by Gould in 1960. Cabanas established the basis of modern sentinel lymph node theory by advocating that the status of the sentinel node should be used as a guide for lymphadenectomy. In 1992, Morton et al introduced lymphatic mapping with blue dye to identify the SLN and demonstrated they could identify the node in 82% of patients with a negative predictive value near 98%. Alex and Krag later used lymphoscintigraphy and a handheld gamma probe to aid in identifying the sentinel node.
Sentinel lymph node biopsy has been used to detect occult nodal metastases in a variety of malignancies including breast cancer and cutaneous melanoma. Its role, however, in cutaneous SCC has yet to be fully elucidated.
Squamous cell carcinoma (SCC) is the second most common malignancy of the skin with 200,000 new cases diagnosed in the United States every year. Although the majority of these tumors are discovered early and cured with local surgery or other ablative modalities, a small subset demonstrate more aggressive biological behavior and are associated with an increased risk of locoregional recurrence, distant metastases, and mortality.
For cutaneous SCC, high-risk tumor characteristics include large size, rapid growth rate, irregular borders, moderate/poor differentiation, perineural invasion, recurrent lesions, sites of prior radiation therapy or inflammation, and immunocompromise. There is not a standard size criteria for high risk SCC: some studies define high risk tumors as those measuring greater than 2 cm on the trunk and extremities, more than 1 cm on the cheeks, forehead, scalp, and neck, and greater than 0.6 cm on the “mask areas” of the face, genitals, hands, and feet. In another study, lesions greater than 2 cm in diameter or 4 mm in depth were considered high risk. Read our article “High Risk Squamous Cell Carcinomas of the Face” for more in-depth information.
Patients with cutaneous SCC with high-risk features have a risk of local recurrence that can be as high as 47%. Rates of regional and distant metastases range between 11 and 47% compared to 2-6% for low-risk lesions. Nodal metastases are associated with a poor prognosis with an expected 5-year survival of 26-34% and 10 year survival of 16%. These sobering statistics underscore the importance of early detection and treatment of SCC.
Although elective treatment of the clinically N0 draining nodal basin with surgery or radiation are reasonable considerations for high-risk disease, each carries the potential for significant morbidity and long-term functional impairment. Sentinel lymph nodes biopsy is an appealing method for accurately staging high-risk SCC with minimal associated morbidity. Early nodal disease can be identified and patients can be selected who may benefit from neck dissection or radiation therapy.
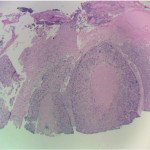
In a recent study, the authors reviewed the literature for cases where sentinel lymph node biopsy was performed for cutaneous SCC with at least one high-risk feature. In these studies, sentinel lymph nodes were successfully identified in 98.5% of cases and the probability of Sentinel lymph nodes positivity was 14.1 % overall with 10.1% being positive in the head and neck and 18.6% being positive in the trunk/extremities. Overall, negative predictive value for SLN biopsy was 97.8% with head and neck cases having a NPV of 100% (no regional nodal recurrences occurred in any patient found to have a negative Sentinel lymph nodes).
When positive sentinel lymph nodes are identified, lymph node dissection is recommended because regional nodal disease is associated with an increased risk of recurrence and decreased survival. However, there are no significant studies showing a survival impact from lymph node dissection in these cases. In one large series of patients from MD Andersen Cancer Center who underwent lymph node dissection for regional SCC nodal disease, 52% had disease recurrence and 75% later developed distant metastases. Further studies are needed to define the role of SLN biopsy in high-risk cutaneous SCC and demonstrate a true survival benefit from undergoing lymph node dissection after a positive SLN biopsy.
Here is a brief video of Sentinel Lymph Node Biopsy performed at Skin Cancer and Reconstructive Surgery Center.