FIELD CANCERIZATION WITH BASAL CELL CARCINOMA
 2012 Radiation Simulation
2012 Radiation Simulation
 Persistent cheek recurrence of BCC at edge of flap
Persistent cheek recurrence of BCC at edge of flap
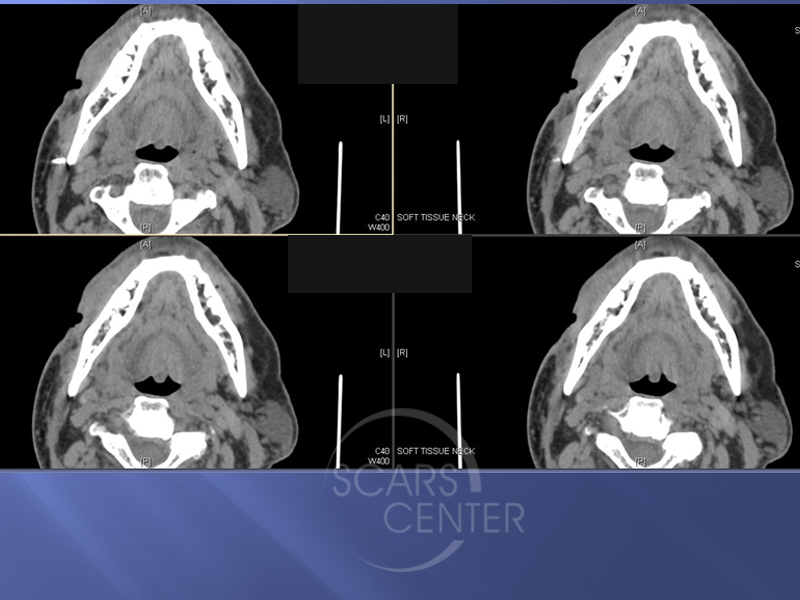
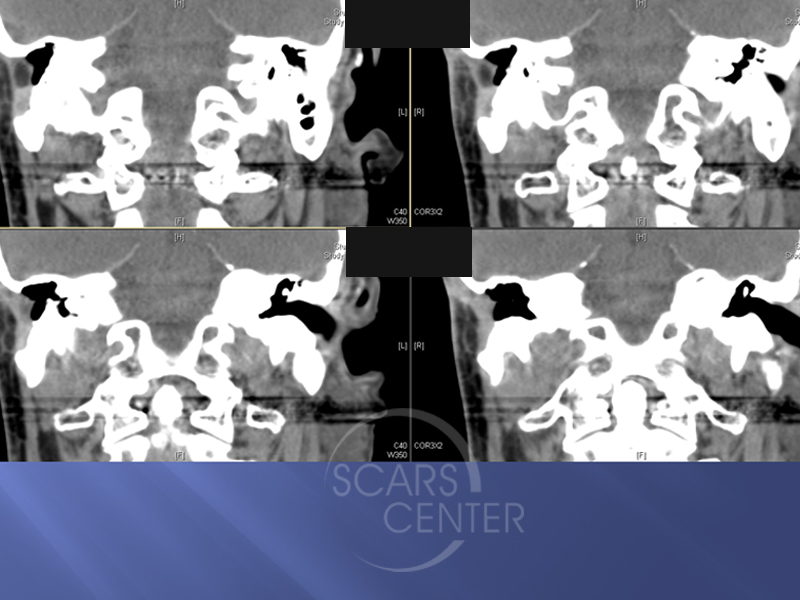 recent CT showing resected right temporal bone with overlying flap and evidence of deep tumor
recent CT showing resected right temporal bone with overlying flap and evidence of deep tumor
HISTORY
This 69-year-old man presented with greater than 25-year history of multiple basal cell carcinomas of the face and neck. His most problematic cancer has been in the right face. The right facial basal cell carcinoma story that we were able to uncover started 11 years ago with wide local resection of right ear and neck basal cell carcinoma. It was excised with positive margins left the resection margin. It was at that point that the cancer became unresectable and all subsequent treatments were either partial or futile. Nine years ago two years after the resection, the patient underwent electron beam radiotherapy to treat multiple recurrent nodules around the scar of the resection from two years ago. This included the area from the ear to the neck on the right side.
Four years later, the patient developed recurrence of what was thought to be squamous cell carcinoma of the ear canal and inferior ear area. He underwent resection of the inferior portion of the ear and the neck and face with again positive margins. The positive margins included infiltrative basal cell carcinoma and not squamous cell carcinoma. The area was covered with a skin graft.
At that point, the patient underwent IMRT radiation to the area due to residual positive surgical margins. A year later, the ear started to drain and osteoradionecrosis of the temporal bone was suspected. As a result, the patient was treated with lateral temporal bone resection and closure with large vascularized myocutaneous flap. Again positive margins were found at the deep aspect of this resection.
At that point, it was accepted that the patient had unresectable basal cell carcinoma. Subsequent treatments were based around recurrences near the flap margins and C&D of the right lower eyelid cheek junction.
The patient has had two courses of vismodegib (Erivedge) two years ago and again this year. The longest course was four months. The patient is not able to continue the medication due to drug tolerance issues.
DISCUSSION
This case is a classic demonstration of a highly aggressive basal cell carcinoma that escapes surgical management many years ago. Despite the residual cancer, the patient has been doing relatively well over the last 11 years. This case also demonstrates living with deeply invasive basal cell carcinoma is possible as the patient is able to maintain activities of daily living and a business.
The subsequent treatment for this patient can only involve oral vismodegib to tolerance. The treatment can be pulsed as the patient is able to tolerate the drug. One of the considerations is to try an alternative Sonidegib (Odomzo). This is another hedgehog signaling pathway inhibitor marketed by Novartis pharmaceuticals. Any surgical management should involve only symptomatic relief of local carcinoma involvement. In this patient, this may involve the treatment of the right lower eyelid retraction caused by scarring and previous C&D procedures.

