About Basal Cell Carcinoma
Basal cell carcinoma (BCC) is the most common form of skin cancer arising from basal cells residing within the dermal-epidermal junction of the skin. This cancer is usually easily detectable as it forms plaques, nodules, or scabs on the surface of the skin. Basal Cell Carcinomas of the skin are the least aggressive skin cancers that we treat in Orange County. These cancers only cause local tissue invasion and some destruction, and almost never metastasize. Basal Cell Carcinoma of the skin are very slow growing as a rule with some lesions taking many months to evolve.
We perform basal cell carcinoma treatment from our Newport Beach clinic. Treatment of these cancers are numerous including curettage, simple excision, Moh’s surgery, and superficial radiotherapy. Other alternative treatments can include topical cancer treatment creams.
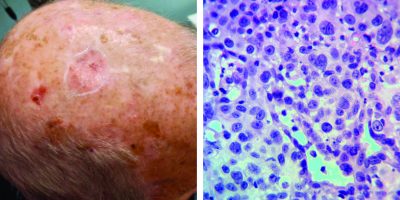
Diagnosis
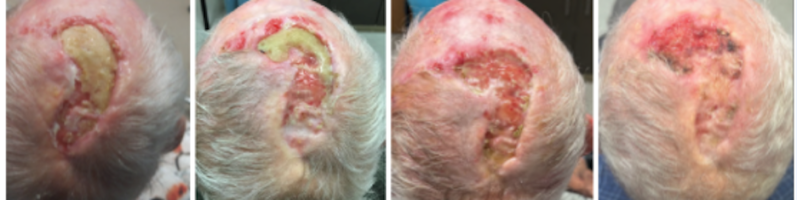
More Complicated BCC
Rarely Basal Cell Carcinoma can be very aggressive infiltrating deeply into tissue. Some BCC’s can invade from skin into bone and cartilage. Some can even penetrate into vital structures such as ear canals and orbit. Although most BCC are visible to the skin, some can grow rapidly and extensively without showing much surface changes. Some rare BCC can be so deeply invasive and infiltrative that surgical treatment is no longer possible. We have had experiences with BCC’s invading cranial cavity, orbit, and maxilla. Some of these require radical soft tissue and bone resection or orbital exenteration. Some BCC’s are simply not treatable surgically.
Related Articles
Management of Non-Healing Lesion
A Case of Mistaken Identity: Porocarcinoma of the Scalp Initially Diagnosed as Basal Cell Carcinoma
Intralesional 5-fluorouracil for Cutaneous BCC and SCC
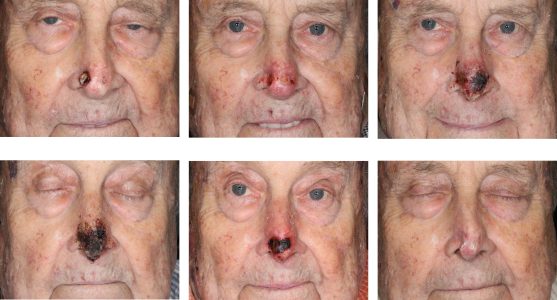
Nasal Open Wound Complication
Recurrent BCC of the External Ear After Radiation
Trichoepithelioma
STAY UP TO DATE
Receive research updates, inspiring stories, healthy living tips and more.
CME ACCREDITED SKIN CANCER CONFERENCE
Earn your CME credits at the SCARS Foundation Monthly Skin Cancer Conference
FOLLOW US
ELEVATING THE STANDARDS OF SKIN CANCER MANAGEMENT.