Management of Non-Healing Lesion
HISTORY
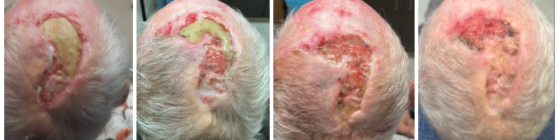
An 85-year-old man with a history of multiple BCC and SCC of the scalp previously treated with radiation and intralesional 5-FU presents with a non healing lesion of the left parietal scalp. Shave biopsy of the left parietal scalp performed on 7/21/21 showed a non specific ulcer with atypical squamous epithelium of the scalp.
DISCUSSION
Chronic wound care can present a challenge for both providers and patients.
With a history of multiple skin cancers, it is important to confirm that non-healing wounds are not malignant. For this patient, the provider may consider multiple, small, scouting biopsies to rule out malignancy in a potentially heterogeneous region.
It is also important to consider the presence of mixed bacterial infection underlying any crusting of chronic wounds. Chronic wounds are susceptible to biofilms that contain microbes which may inhibit healing. Silver ions, salts, and colloidal preparations can be used to prevent the growth of gram-positive and gram-negative bacteria in these biofilms. Products such as calcium alginate can be used to absorb moisture off the wound surface, which limits biofilm formation.
Alternatively, some wounds without crusting are best kept “wet” and duoderm dressings are helpful. Duoderm offers an outer film that provides a waterproof barrier, a foam layer for thermal and mechanical protection, and a honeycomb hydrocolloid matrix to keep a damp environment. The hydrocolloid matrix helps absorb exudate, keep nerve endings moist and unagitated, and promote wound healing by increasing epithelization, enhancing collagen synthesis, and promoting macrophage involvement. The dressing can be worn for up to 7 days at a time, making wound care relatively low maintenance for patients and their caretakers.
Wet to dry dressings offer another option and provide mild debridement. Debridement serves to remove exudate thus preventing scabbing and minimizing biofilm on the wound. Woven gauze soaked in Aquaphor and/or diluted acetic acid (vinegar) provides an initially wet dressing that then dries on top of the wound. When the gauze is removed, some of the unhealthy wound tissue and exudate is removed as well. Vinegar is a useful product that can help prevent and limit proliferation of pseudomonas bacteria. If vinegar is not needed, Aquaphor alone can be applied to moisten the gauze which will also dry up and provide mild debridement when removed. Frequent dressing changes are the hallmark of this strategy.

The ultimate wound healing device is the wound VAC (short for vacuum assisted closure). A wound VAC decreases air pressure around a wound to improve healing. Wound VACs gently pull fluid from the wound which reduces swelling and reduces opportunity for bacteria colonization. They also help pull the edges of the wound together and promote new tissue growth. A wound VAC utilizes a gauze or foam dressing directly on the wound, an adhesive film to seal the dressing on the wound, and a drainage tube that connects the wound to a portable vacuum pump. The dressing must be changed every 24 to 72 hours.
