Melanoma within recurrent MIS

Resection margins of melanoma in situ. Reconstruction of the cheek portion of the defect with a nasolabial fold island advancement flap, reconstruction of the nasal alar component with a skin graft. Recurrent invasive melanoma 6 years later.
HISTORY
73-year-old woman presents with 1-year history of recurrent pigmented lesion of the right nasal ala found to be invasive melanoma with 0.5 mm invasion. Patient’s history began 9 years ago in 2009 with excision of a melanoma in situ and skin graft closure. In 2012, pigmentation adjacent to the graft site was found to have junctional severely atypical melanocytic proliferation. The lesion was excised at that point with 5 mm margins with finding of melanoma in situ and clear margins. Additional margins were taken at the time of reconstruction with no residual melanoma found.
DISCUSSION
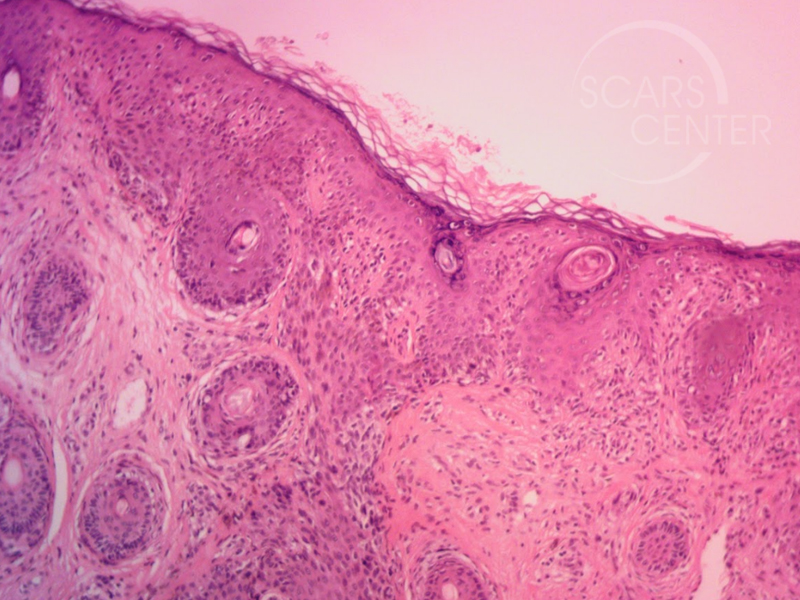
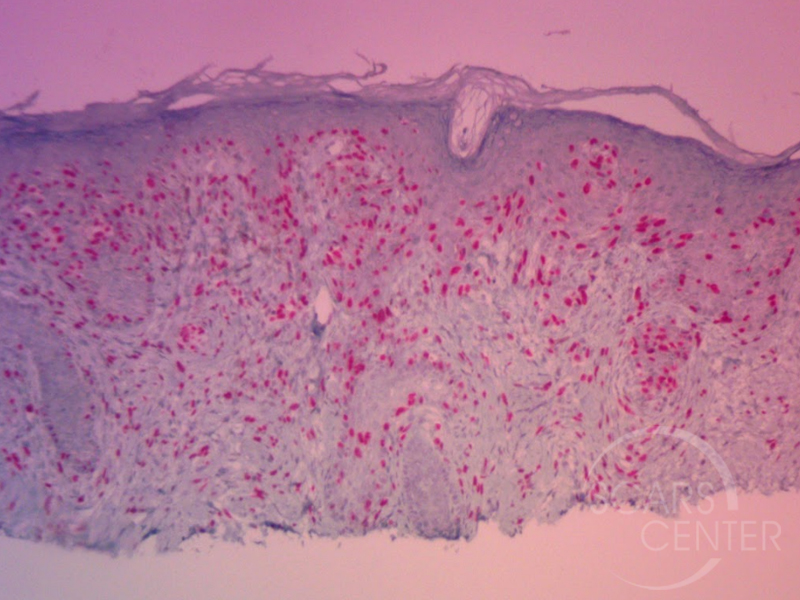
On histology, this invasive melanoma exhibits desmoplastic features extending to the deep margin of the shave biopsy. This tumor has to be treated as a higher risk melanoma with depth of invasion to be assumed greater than 1 mm. This assumption of deeper invasion is due to involvement of the deep margin of the shave biopsy. Desmoplastic melanomas have a tendency for neurotropic behavior making the resection margins much greater. In addition, desmoplastic melanomas frequently lack dark pigmentation, making their spread undetectable and presenting as larger lesions.
Mapping of the margins of this cancer is particularly useful in this patient. The location in cosmetically sensitive anatomic region, the nose, will result in a complex defect requiring a complex reconstructive plan.The desmoplastic features of the melanoma limit the usefulness of visual assessment of the margins. Thus, pre-operative mapping provides the reconstructive surgeon and the patient with the expected defect size and a specific reconstructive plan. Mapping is best performed with punch biopsies. Reflectance confocal microscopy is a noninvasive mapping alternative for assessment of mostly flat areas.
Sentinel lymph node assessment should be considered in this patient based on the assumption of deeper involvement of the tumor. It can be performed at the same surgical visit as the mapping biopsies.
Prognosis of desmoplastic melanoma is variable. Some studies have suggested a better prognosis for desmoplastic melanomas relative to the non-desmoplastic melanomas, despite findings of deeper invasion at time of presentation. A large patient review from 2010 found that only wide local resection and adjuvant radiation therapy correlated with survival. Breslow’s depth, nodal positivity, and ulceration did not predict survival. Post-operative radiation therapy is indicated in this patient to improve survival.
