Lethal Squamous Cell Carcinoma of the Forearm in a Lung Transplant Recipient
HISTORY
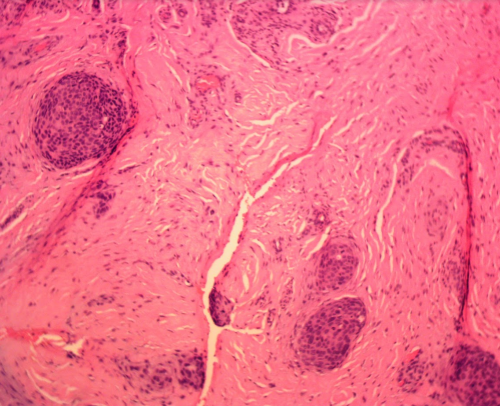
A 71-year-old lung transplant recipient presented with a recurrence of left dorsal forearm and wrist Squamous Cell Carcinoma (SCC) after Mohs excision in 2016 performed elsewhere. The patient underwent Mohs excision with clear margins and additional deeper wide local resection with no carcinoma identified.
Patient was referred for radiation oncology evaluation, but he was not treated with radiation at that point. SCC recurred 8 months later in 10-2017. Mohs surgery again achieved clear margins on 11-21-17. But additional deeper margin taken during reconstruction showed deeply invasive squamous cell carcinoma. Patient continued treatment at City of Hope Orthopedic Oncology where they found metastases in the axillary lymph nodes. He underwent bone sparing forearm resection and radiation to the forearm and the axilla. His axilla radiation course was complicated by lung rejection that was successfully treated with additional immunosuppression. The patient succumbed afterward to an aggressive pulmonary fungal infection that arose as a consequence of immunosuppression.
DISCUSSION
High-risk forearm squamous cell carcinoma has to be evaluated with axillary imaging for lymphadenopathy or a possible sentinel lymph node biopsy of the axilla. Wide local resection with post-op radiation is also indicated. In this patient, wide local resection of forearm soft tissue was performed while sparing the bones. Additional local site radiation was required. Radiation of upper extremities can result in fibrosis, joint stiffness, and edema, adversely affecting function.
Our patient’s demise was a link of complications starting with radiation pneumonitis caused by axillary radiation. The radiation pneumonitis triggered a rejection response to the lung transplant. The higher dose immunosuppression was complicated by a fungal infection to which the patient succumbed.
Although we had a high index of suspicion of deeper involvement after the second Mohs excision, we could not validate that suspicion with deeper margin resection. It took a second recurrence to find the cancer skip area extending between the radius and ulna. In hindsight, the higher index of suspicion at the time of the first recurrence should have resulted in local radiation to the area.