Peri-Auricular Neoplasm – Deception in Waiting
Peri-auricular subcutaneous lesions can be deceptive. These neoplasms have a higher risk of being non-dermal-related tumors than neoplasms of other areas of the face. Attempts at excision without consideration of a differential diagnosis can often lead to tumor compromise. Over the last several months, SCARS Center has treated several tumors previously excised partially by other physicians, prompting this subject review.
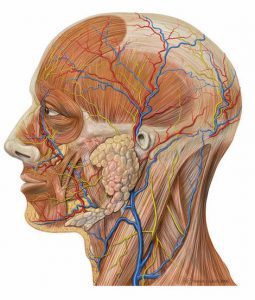 The appeal of excision of subcutaneous tumors in this area arises from the fact that peri-auricular tumors do not pose a risk to vital underlying structures such as nerves and major vessels for the most part. However, even that appeal needs to be tempered by proximity of superficial temporal vessels in the superior pre-auricular area. The parotid gland is the major anatomic structure underlying most peri-auricular pathologies.
The appeal of excision of subcutaneous tumors in this area arises from the fact that peri-auricular tumors do not pose a risk to vital underlying structures such as nerves and major vessels for the most part. However, even that appeal needs to be tempered by proximity of superficial temporal vessels in the superior pre-auricular area. The parotid gland is the major anatomic structure underlying most peri-auricular pathologies.
It is often the pathologies of the parotid gland that can be confused with dermal and subcutaneous lesions. The most common is pleomorphic adenoma – a benign neoplasm of the parotid salivary gland. 85% of all parotid gland neoplasms are actually benign. In addition to pleomorphic adenomas, a less common Warthin’s tumors (cystadenoma lymphomatosum) represents another benign parotid pathology and tends to be multiple or bilateral.
The problem with treating a pleomorphic adenoma as a subcutaneous cyst or a dermal nodule is the seeding of the surgical field with the tumor. Although these tumors appear encapsulated, they have microextensions beyond the capsule. Thus, removal of pleomorphic adenomas by enucleation results in recurrence. When approached surgically as a subcutaneous lesion, the procedure is often abandoned and the skin incisions closed due to the depth of tumor extension. Subsequent definitive treatment in these cases involves removal of the tumor with overlying skin and fascia assumed to be seeded with tumor cells.
Other cases we had seen at SCARS Center involve attempts at excision of pre-auricular lymph nodes with metastatic carcinoma. Some lymph nodes in the upper part of pre-auricular area are quite superficial and can appear as cysts. Lymph nodes with extracapsular extension of the cancer have a tendency to be adherent to surrounding structures. Attempts at excision of these tumors often results in procedure termination and skin closure. This can be treated after the fact, but requires a wider surgical resection than would have been necessary if the incision had not been attempted. Enlarged lymph nodes in the peri-auricular area require evaluation of the source of the lymphatics – scalp, lateral forehead, and lateral orbit.
 A third pathology that requires caution is the congenital pre-auricular cyst associated with a pre-auricular pit. These cysts can appear over 1 cm anterior to the root of the helix. The origin of these cysts is the pit at the root of the helix which is connected by a sinus tract. Excision of the cyst requires removal of the sinus tract, the pit, and occasionally the cartilage of the helical root. Failure to do so can result in recurrence. These cysts have a tendency to get infected making subsequent surgical treatment of a fibrotic
A third pathology that requires caution is the congenital pre-auricular cyst associated with a pre-auricular pit. These cysts can appear over 1 cm anterior to the root of the helix. The origin of these cysts is the pit at the root of the helix which is connected by a sinus tract. Excision of the cyst requires removal of the sinus tract, the pit, and occasionally the cartilage of the helical root. Failure to do so can result in recurrence. These cysts have a tendency to get infected making subsequent surgical treatment of a fibrotic

field challenging.
Rare disasters in waiting are vascular neoplasms of the superficial temporary artery – aneurysms, pseudoaneurysms, and arteriovenous
malformations. Although the temporomandibualr joint lies deep in the pre-auricluar space, its neoplasms can also present superficially. These include osteochondroma, synovial cyst, hemangioma, and others. Superficial sensory branches of the great
auricular nerve can be a source of neuromas and neurofibromas in the area as well.
Another peri-auricular pathology includes first branchial cleft cyst. It can present superficially in the lower portion of the peri-auricular area or at the inferior portion of the ear canal. The congenital sinus tract of these cysts can extend deep into the parotid gland or neck. These lesions require comprehensive pre-operative imaging.
Peri-auricular cysts and dermal nodules should be approached with suspicion and some trepidation. Differential diagnoses are multiple, and treatment can be more than skin deep.
