A Case of Mistaken Identity: Porocarcinoma of the Scalp Initially Diagnosed as Basal Cell Carcinoma
History
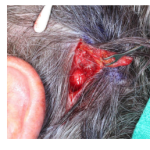
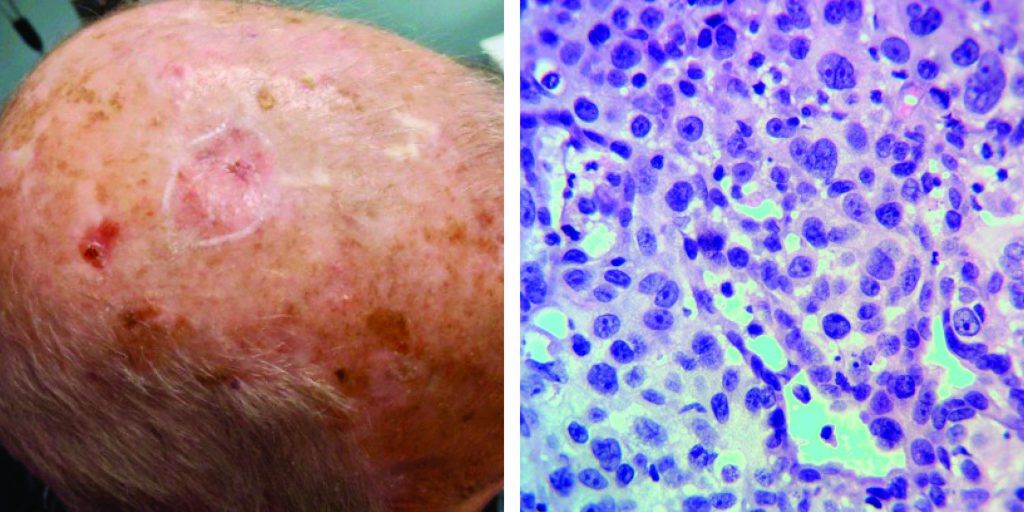
A 72-year-old man presented with a 2 year history of right anterior scalp lesion. The lesion was previously treated by an outside physician with cryosurgery multiple times over the course of 1 year. After a lack of resolution, the lesion was biopsied resulting in a diagnosis of basal cell carcinoma. No further treatment was pursued and six months later the patient underwent a second biopsy that showed poorly differentiated porocarcinoma. Upon diagnosis with porocarcinoma, the patient presented to our office for further evaluation and treatment. He underwent repair with a rotation flap.
Discussion
Poromas, aka eccrine poromas, are benign sweat gland tumors that generally present as solitary, vascular-appearing papules/nodules with or without ulceration and bleeding. They are classically found on the palms and soles, as these sites contain the highest concentration of eccrine glands.They arise from the acrosyringium, the intraepidermal portion of the eccrine duct.
Porocarcinoma, aka eccrine porocarcinoma, is a rare cutaneous neoplasm representing 0.005-0.01% of all cutaneous tumors. Up to 50% of porocarcinomas arise from their benign counterparts, likely from chronic uv light exposure and/or immunosuppression. Roughly half of the cases of porocarcinoma develop on the lower extremities, followed by the trunk, and head and neck regions. Clinically they may develop as papules, nodules, or plaques.
Diagnosis is usually made via biopsy. Histopathologic findings include nuclear atypia, increased mitotic activity, necrosis, and intraepidermal polygonal tumor nests of varying sizes. Tumor borders may be infiltrative, pagetoid, and/or pushing. Immunohistochemical stains used in detection of porocarcinoma includes CD117, carcinoembryonic antigen (CEA), cytokeratin (CK) (pancytokeratin and CK5/6), epithelial membrane antigen (EMA), p53, and p63.
Treatment is necessary due to its aggressive nature with 20% metastatic and recurrent rate at diagnosis. Mortality is 10% although if nodal involvement occurs, mortality approaches 67%. Mean survival with distant metastatic disease is roughly 3-24 months.