Evaluation of Longitudinal Melanonychia
HISTORY
An 84-year-old woman with a history of melanoma of the left upper back presents with an 11 month h/o left great toe discoloration. Biopsy of left great toe was performed on 08/05/2019. Previous h/o discoloration of the right fifth toe was biopsied and was negative for malignancy.

DISCUSSION
What is the cause of melanonychia striata? What are the best way to clinically differentiate longitudinal melanonychia from melanoma? How should concerning lesions be biopsied? Melanonychia striata, aka longitudinal melanonychia, is a common finding in dark-skinned individuals (Fitzpatrick phototypes IV-VI). Often a benign finding, it is vitally important to clinically differentiate it from subungual melanoma.
The differential diagnosis is broad and includes benign melanocytic activation of the nail matrix (caused by medications, infections, irradiation, trauma, pregnancy, dermatologic, endocrine, and genetic disorders, etc.), as well as melanocytic hyperplasia of the matrix. This includes benign melanocytic nevi, lentigo, nail apparatus/subungual melanoma, subungual pigmented Bowen’s disease, and subungual squamous cell carcinoma.
When compared to benign melanonychia striata, subungual melanoma usually appears abruptly, grows rapidly, occurs after middle age, involves a single digit, and usually the patient lacks a family history melanonychia striata. Clinically the melanonychia of the melanoma may become darker, have color variegation, blurry lateral borders, irregular elevation or dystrophy of nail plate, a pigment band width of >3mm, proximal widening (a triangular shape) and/or a positive Hutchinson sign.
Hutchinson sign, periungual extension of brown-black pigmentation from longitudinal melanonychia onto the proximal and lateral nail folds, although not pathognomonic for subungual melanoma, is highly suggestive of its presence.
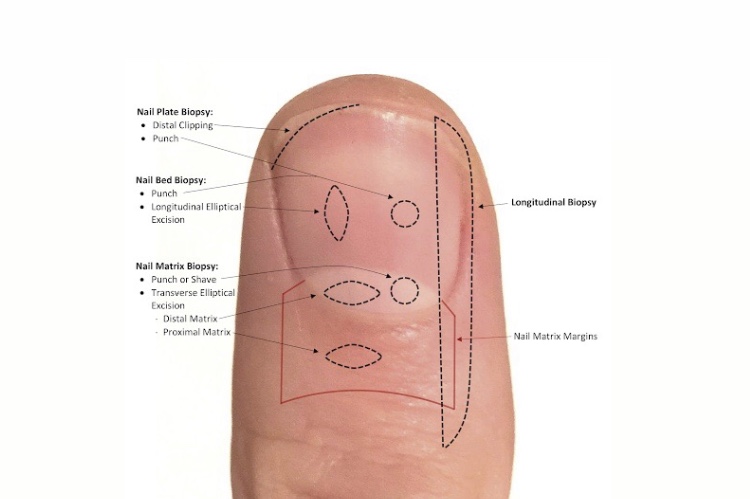
Biopsy for melanonychia should be performed at the nail matrix, where the melanocytes reside. The proximal nail fold should be reflected prior to assessing for the proper biopsy site. Best results are usually achieved after avulsion of the nail plate. (see photo) The excisional biopsies should be oriented horizontally in the matrix to prevent onychodystrophy in the future. In some cases, such as the one presented here, a longitudinal / vertical excision can be performed to evaluate the full extent of the matrix and nail bed. But this can only be performed in the lateral / medial periphery of the matrix to avoid nail splitting and dystrophy. It is best done by an experienced dermatologist / dermatologic surgeon.
*Leung AKC, Lam JM, Leong KF, Sergi CM. Melanonychia striata: clarifying behind the Black Curtin. A review on clinical evaluation and management of the 21st century. Int J Dermatol. 2019 Apr 21. doi: 10.1111/ijd.14464. [Epub ahead of print]