Recurrent Extensive Basal Cell Carcinoma of Forehead





HISTORY
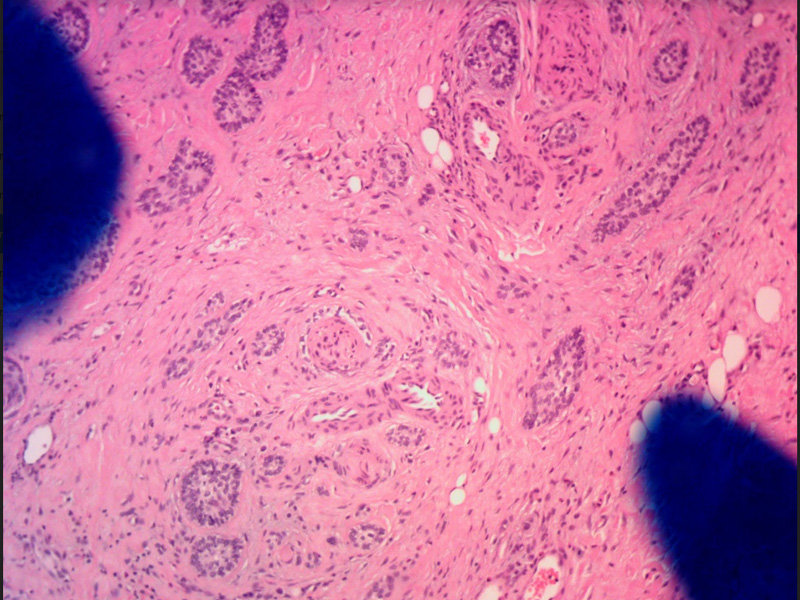
68-year-old man presented with a recurrent right forehead basal cell carcinoma. The carcinoma was previously treated with Mohs excision in 2002 and 2009. The recurrence appeared initially as superficial and was treated successfully with topical imiquimod. Deep recurrence became evident many months later. Morphology of the basal cell carcinoma was infiltrative with metatypical features.
Mohs was performed on 6/26/2017 with residual positive inferior margin. Clear margins were achieved after 3 additional wide local resections and formalin fixed histopathology. Focal perineural invasion was found at the supraorbital nerve.
DISCUSSION
Recurrent extensive basal cell carcinoma of the forehead. This extensive basal cell carcinoma of the forehead represents a unique approach were used at scar center combining precision of Mohs excision and effectiveness of wide local resection. This particular patient’s basal cell carcinoma was extensively invasive with deep infiltration along the periosteum and subcutaneous spread. Mohs defined the cutaneous spread of the tumor and cleared the superior two thirds of the carcinoma. The inferior one third and the periosteal spread of the carcinoma was left for intraoperative surgical resection. Incomplete Mohs excision is not viewed as negative in our center. In fact, it can be viewed as a gift to the oncologic surgeon where majority of the margins are defined and the nature of additional margins can be inferred. Thus, instead of resecting unnecessary large margins all around the cancer only the most critical aspect is addressed by the oncologic surgeon. In this patient, the critical margin was in the eyebrow and eyelid including the orbital margins. This was difficult to achieve under local anesthesia utilizing Mohs surgery and was left for operating room resection. Stat permanent margin evaluation was performed with the help of Laguna Pathology Medical Group with the results available less than 24 hours after resection of margins. This particular patient had three additional wide local resections done two days apart to achieve clear margins. This combination of Mohs excision with operating room-based wide local resection provides both the precision and tissue sparing economy of Mohs surgery and oncologic effectiveness of operating based surgery. An additional point for this patient is the ability to perform bone margin. Because of such close involvement of the periosteum by this highly infiltrative basal cell carcinoma, thin bone margin was resected utilizing 5 mm osteotomes. The bone was submitted in sections to evaluate for possible presence of residual carcinoma. This achieved both an additional oncologic margin of clearance for the basal cell carcinoma as well as confirmation of clear margins. We utilized porcine xenograft for coverage of exposed bone during the two-week of bone exposure of this patient. The bone was exposed while the margins were cleared with serial wide local excisions. Porcine xenograft served as a biological dressing. Its adherence to biological tissue is remarkable as the bone incorporated porcine xenograft tightly as a periosteum. When reconstruction was performed, the porcine xenograft was peeled off the bone. The peeling off felt as if the periosteum was removed and underneath the xenograft, small lacunae of blood supply were seen as the bone bled through these well vascularized openings. Porcine xenograft serves as a biological dressing and protects the bone from desiccation and loss of superficial blood supply.


