Dermatofibroma to Dermal Sarcoma: The Spectrum of Dermal Spindle Cell Tumors
HISTORY
A 54-year-old woman with no history of skin cancers presented with 4 month h/o growing left cheek nodule. After a shave biopsy that suggested a dermatofibroma, the tumor progressed to ulceration .
A 74-year-old man presented with a 2 month h/o bleeding, ulcerated nodule of left antitragus. He has a history of several skin cancers. The tumor was diagnosed as atypical fibroxanthoma (AFX) on a shave biopsy.

DISCUSSION
These two cases represent different parts of the spectrum of “benign” mesenchymal spindle cell tumors. The woman’s cheek diagnosis was upgraded to atypical fibrous histiocytoma (AFH) bordering on an atypical fibroxanthoma (AFX) after tumor excision. The tumor was excised with 1.5 cm margin.
The man’s ear tumor was resected with underlying cartilage to assess for invasion. Spindle cells closely approached the perichondrium without invasion. Consideration of an early pleomorphic dermal sarcoma (PDS) was recommended. The patient underwent sentinel lymph node biopsy, which was negative.
Literature review of the subject identified the spectrum of disorders with a risk of recurrence and metastases. Although classification appears to rigidly separate AFH, AFX, and pleomorphic dermal sarcoma (PDS), these are relative terms. In fact, in many studies, the tumor is reclassified based on subsequent clinical behavior. Tumor diagnosed as a classic AFX initially is reclassified as PDS after metastases are discovered. However, invasion of the subcutis and dermis are the demarcation for the pathologist to label the tumor as a PDS.
A strong argument can be made that all such tumors require a full thickness evaluation with permanent FFPE histology. Given that Mohs surgery is so effective in clearing the margins and minimizing tumor recurrence, where would permanent histology fit? A compromise solution is resecting a full thickness of the central tumor for FFPE permanent histology followed by Mohs levels for margin clearance. Studies have shown that 2 cm margin is frequently needed to histologically clear the tumors.
At SCARS Center we also utilize sentinel lymph node biopsies for tumors approaching the PDS classification – subcutis invasion.
Finally, given the bland H&E appearance of these tumors, robust immunohistochemistry is required to differentiate these from other spindle cell tumors. The differential diagnoses include spindle cell and desmoplastic squamous cell carcinomas, spindle cell melanoma, leiomyosarcoma, cutaneous angiosarcoma, and dermatofibrosarcoma protuberans (DFSP).

(click image to enlarge)
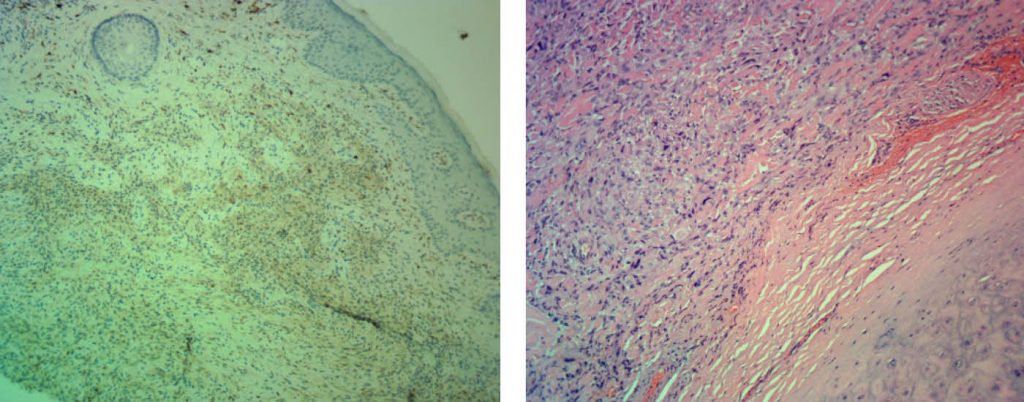
Right: Ear AFX abutting perichondrium – an early pleomorphic dermal sarcoma.

