Lower Leg Radiation Ulcer




HISTORY
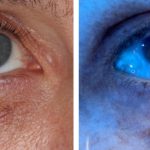
85-year-old man presented in March 2015 with a multi-year history of a non-healing right lower leg lesion. Shave biopsy found squamous cell carcinoma in situ with focal areas of early invasion. Superficial radiotherapy was prescribed at 50 kvp 5 days per week for 5 weeks ending in July 2015. Minor skin erosion present 3 weeks after treatment cleared up by the two month follow up.
Two years later, on 4/10/2017, patient presented with redness and pain of the right lower leg with a 1 cm superficial ulceration. The wound was managed with antibiotics initially, then collagenase cream (Santyl), and foam wound dressing. Two wound debridements were performed, and negative pressure wound therapy was initiated on 6/21/2017 with excellent granulation response. Patient also underwent saphenous vein ablation to minimize leg edema. Finally, dermal collagen xenografts were applied to the wound to facilitate final stages of healing.
DISCUSSION
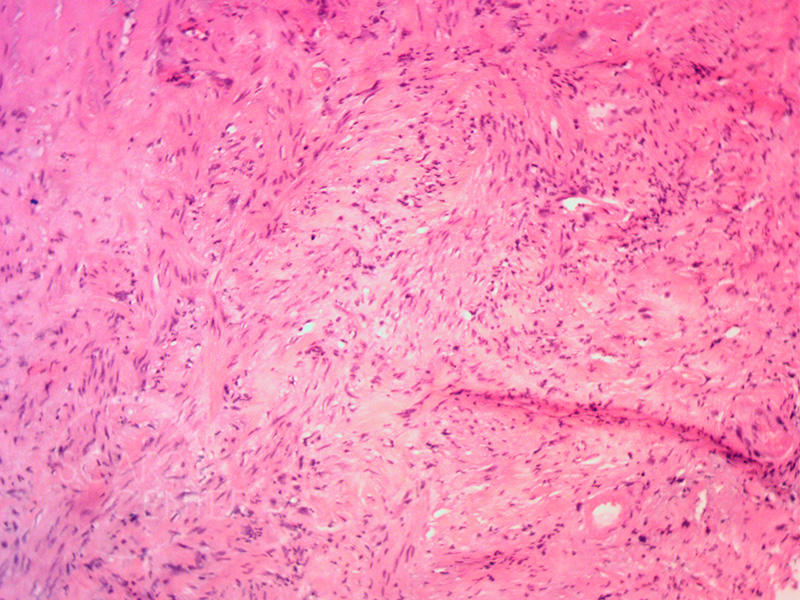
There are five basic elements of chronic wound treatment. These are routinely applied to treatment of radiation ulcers. This discussion deals specifically with delayed post-radiation ulceration that can occur as early as six months to many years after completion of radiation therapy. The causes of post radiation breakdown and ulceration include relative ischemia of the radiated tissues, local tissue tension caused by such factors as edema, local minor injury introducing localized bacteremia, and poor immunocompetence of the individual due to systemic factors. Each of these factors can worsen blood supply of the radiated tissue even further. At a certain point, as the blood supply diminishes, the local tissue can necrose creating a pocket for bacterial contamination. Once this area becomes infected, break down is inevitable. In our experience, the most common immediate cause of radiation ulcer is acute edema whether caused by systemic illness or localized extremity swelling due to venous insufficiency.
Treatment of delayed radiation ulcers or chronic lower extremity wounds first involves treatment of acute infection. The second important element is debridement of ischemic or necrotic tissue. This is initially performed conservatively and may need to be repeated once or twice to achieve complete debridement of all ischemic tissue.
Local wound care involves avoiding wetness and fluid collection within the depth of the wound. This is achieved with wound sponge dressings that effectively wick off extra drainage in the wound surface. A Wound-Vac is an even more effective way of removing extra tissue fluid of the wound. Unfortunately, the patient is burdened with carrying a small electric pump to maintain the negative pressure with intermittent suction on the occlusive sponge dressing.
Use of collagenase cream avoids early scar inflammation in the wound that would inhibit neovascularization. Saphenous vein ablation is occasionally performed if vascular studies find that the patient has incompetent venous system. This decreases chances of peripheral edema. Finally, xenograft dermal collagen application encourages stronger wound formation.
In some cases, hyperbaric oxygen therapy is used to encourage neovascularization. This is a highly burdensome treatment involving daily high pressure oxygen chamber incubation (dive) lasting up to an hour. Hyperbaric oxygen treatment or HBO therapy is done five days a week for two to four weeks. Although HBO has been shown to promote neovascularization, no direct evidence exist that HBO therapy helps with radiation ulcers of the extremities. In our opinion given the life-changing nature of this treatment, and its lack of proven efficacy, HBO therapy should be the option of last reserve.