Left Cheek Atypical Spitzoid Nevus
HISTORY
23-year-old woman presents with lifelong history of left cheek mole changing recently. Biopsy in 8/2017 showed compound nevus with severe atypia with spitzoid features. Excision was performed on 2-9-18. The patient a history of atypical mole of the left back removed in 2017.

Cheek Atypical Spitzoid Nevus, 2 ½ weeks post excision
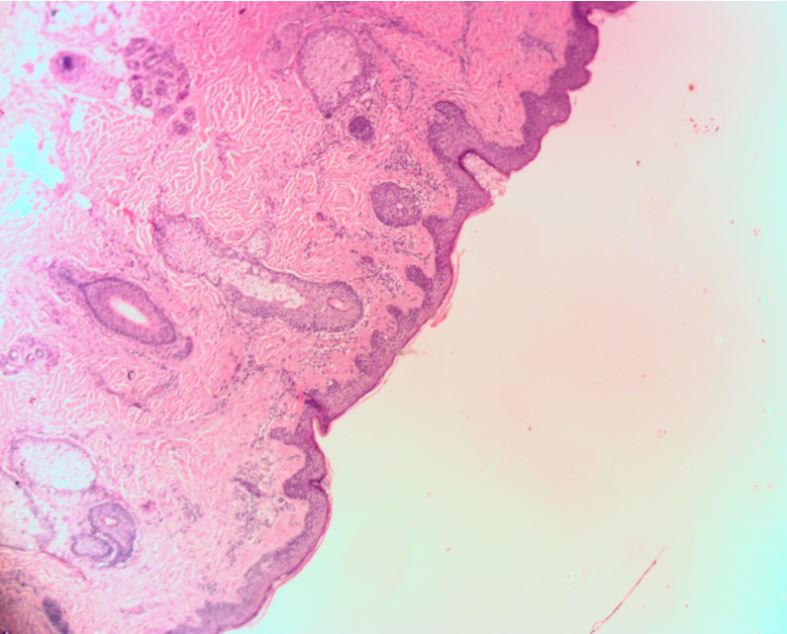
Atypical spitzoid nevus: cytologic atypia of nevomelanocytic cells, arranged in a haphazard configuration, some exhibit spitzoid features.
DISCUSSION
Spitz nevi are are spindle / epithelioid cell nevi or tumors that are predominantly identified in younger age groups and pose a diagnostic and therapeutic challenge. Three classification categories exist:
- Classic Spitz nevus (CSN) – without atypicality
- Atypical Spitz tumor (AST)
- Spitzoid malignant melanoma (SMM)
Unfortunately, pathologic diagnosis discordance plagues these lesions. Even expert dermatopathologists fail to agree on objective criteria to classify each nevus in a subtype. In many cases, even malignant diagnoses cannot be agreed upon.
Malignant Spitz nevi have been described as juvenile malignant melanomas because the lesions are not fatal despite frequent lymph node metastases. Some studies have found that up to one half of patients treated with lymph node biopsies had lymph node metastases. An impressive review of Massachusetts General Hospital records over the course of 30 years found no lethality from any Spitz tumors. Mean follow up period was 9 years. The review included 144 cases, roughly equally split between CSN and AST, including 13 Spitz-associated melanomas (10 SMM’s and 3 melanomas arising in Spitz nevi). Interestingly, 5 of 14 (40%) sentinel lymph node biopsies performed found metastases (1 of 7 AST’s, 3 of 7 SMM, and in 1 melanoma arising in Spitz nevus). There were no distant metastases or deaths from Spitz nevi.
Another notable finding of the Mass General Study was the 8-fold increase in risk of melanoma in patients with either classic Spitz nevi (CSN) or atypical Spitzoid tumors (AST). The authors raise the hypothesis that the early presence of Spitz tumors may be a possible risk marker for subsequent melanomas. So, it makes sense to treat Spitz nevi as any other dysplastic nevus with complete but conservative excision and long term surveillance for new onset melanomas. The margin of excision should be 2-5 mm.
Sepehr, A, Chao, E, Trefrey B, et al. (2011). Long-term Outcome of Spitz-Type Melanocytic Tumors. Arch Dermatol, 147(10), 1173–1179. doi:10.1001/archdermatol.2011.170
Murphy, M, Boyer J. D., Stashower M. E., Zitelli, J.A. (2002).The surgical management of spitz nevi. Dermatologic Surgery, 28(11), 1065-1069.
